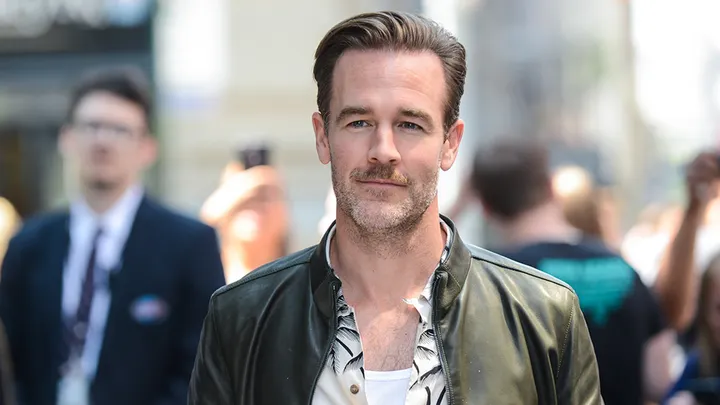
Health experts are urging younger adults to pay attention to colorectal cancer risks and screening after actor James Van Der Beek died at 48 following a battle with colon cancer, a death that has renewed attention on the disease’s rising toll in people under 50.
Van Der Beek, best known for “Dawson’s Creek,” had previously disclosed that he was diagnosed with stage 3 colorectal cancer after a colonoscopy and later spoke publicly about noticing subtle changes in bowel habits before the diagnosis.
Colon cancer under 50 is now the leading cancer killer in that age group, ACS says
New research highlighted by the American Cancer Society found colorectal cancer had become the leading cause of cancer death among Americans under 50, driven by an increase in colorectal cancer mortality while deaths from other major cancers fell over the same period.
The ACS said colorectal cancer mortality in people under 50 rose by about 1.1% per year since 2005, a trend that has pushed the disease from the fifth-leading cancer killer for this age group in the early 1990s to first in recent years.
Symptoms can be subtle, and some people have no early warning signs
Clinicians note that colorectal cancer can develop without obvious symptoms, especially in earlier stages. When symptoms appear, they may include persistent changes in bowel habits, blood in stool, abdominal pain, unexplained weight loss, and fatigue that can be linked to anemia.
Because symptoms can overlap with common digestive issues, medical groups emphasize that persistent changes—especially when new or worsening—should be evaluated by a clinician.
Screening guidance starts at 45 for average-risk adults
US screening recommendations generally advise that adults at average risk begin regular colorectal cancer screening at age 45. The US Preventive Services Task Force recommends screening from ages 45 to 75, with individualized decisions for ages 76 to 85.
The American Cancer Society similarly recommends that people at average risk start screening at 45, using either stool-based tests or visual examinations such as colonoscopy, with follow-up colonoscopy after a positive non-colonoscopy test.
Researchers continue to study what is driving the rise
Experts say established risk factors include family history, obesity, smoking, heavy alcohol use, inflammatory bowel disease, and diets high in red and processed meats, but many younger patients do not fit traditional profiles—one reason researchers continue investigating additional contributors.
A recent study from Mass General Brigham reported an association between higher intake of ultra-processed foods and increased risk of colorectal cancer precursor polyps in younger women, adding to evidence that diet may play a role in early-onset disease.
The renewed attention is also highlighting gaps in screening, as public health groups and clinicians emphasize that earlier detection can identify and remove precancerous polyps and improve outcomes when cancer is found.